This post may contain affiliate links which means I may receive a commission for purchases made through links. As an Amazon Associate I earn from qualifying purchases. I will only recommend products that I have personally used! Learn more on my Private Policy page.
Seborrheic dermatitis is a common, chronic inflammatory skin condition that affects people of all ages and ethnicities. It is characterized by lesions in areas rich in sebaceous glands, such as the scalp, face, ears, and chest. Although it is not life-threatening, seborrheic dermatitis can cause discomfort and embarrassment for those who suffer from it.
Understanding Seborrheic Dermatitis in Diverse Populations
By reading this article, you will learn:
– The prevalence, clinical features, and treatment options for seborrheic dermatitis in different age groups, populations, and medical conditions
– The challenges and potential differences in diagnosis and treatment for people with skin of color
– The main treatment options and tips for managing seborrheic dermatitis in diverse populations
What is Seborrheic Dermatitis?
Seborrheic dermatitis is a skin condition that causes red, scaly patches on the skin. The patches are often itchy and can be found on the scalp, face, ears, and chest. Seborrheic dermatitis is not contagious, but it can be chronic and difficult to manage.
Seborrheic Dermatitis in Different Age Groups and Populations
Seborrheic dermatitis can affect people of all ages, from infants to the elderly. The clinical features of seborrheic dermatitis may vary depending on the age of the patient. In infants, seborrheic dermatitis is commonly known as cradle cap. It usually appears as thick, yellowish scales on the scalp and may spread to the face, neck, and diaper area. Cradle cap usually resolves on its own within a few months but may require treatment if it causes discomfort to the infant or becomes infected.
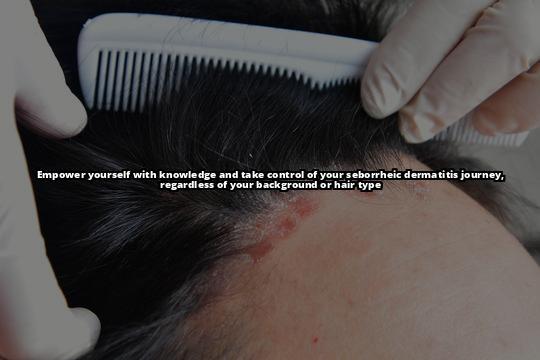
In adults, seborrheic dermatitis usually affects the scalp, face, and chest. It may appear as red, scaly patches that are itchy and flaky. In some cases, seborrheic dermatitis may also affect the ears, eyebrows, and folds of skin around the nose and mouth. The severity of symptoms may vary, but seborrheic dermatitis is usually a chronic condition that requires ongoing management.
In the elderly, seborrheic dermatitis may be more severe and difficult to manage due to age-related changes in the skin. Elderly individuals may also be more susceptible to other medical conditions that can exacerbate seborrheic dermatitis symptoms, such as Parkinson’s disease or dementia. Pregnant women may also be more susceptible to seborrheic dermatitis due to hormonal changes that affect the skin.
Seborrheic Dermatitis in People with Skin of Color
Seborrheic dermatitis can present differently in people with skin of color, making it challenging to diagnose and treat. In people with darker skin tones, seborrheic dermatitis may appear as dark patches or hyperpigmentation. It may also be more severe and resistant to treatment due to the thicker and more sensitive nature of the skin.
The role of the skin microbiome and environmental factors in seborrheic dermatitis pathogenesis and treatment response is also an area of interest in research. More recent research shows that seborrheic dermatitis is associated with a shift in the skin microbiome, with a decrease in bacterial diversity and an increase in fungal colonization. This dysbiosis has been linked to seborrheic dermatitis, and controlling the skin microbiome could help treat and prevent the condition.
Seborrheic Dermatitis in People with Other Medical Conditions
Seborrheic dermatitis can also manifest differently in patients with other medical conditions. For example, a study published in BMC Dermatology found that patients with Parkinson’s disease have a higher prevalence of seborrheic dermatitis, and the dominant species of Malassezia in seborrheic dermatitis patients with Parkinson’s disease was M. globosa. The study suggests that Malassezia density and infection may contribute to the development of seborrheic dermatitis, and treatment with L-dopa, an anti-Parkinson’s agent, may also have an effect on seborrheic dermatitis.
Patients with HIV/AIDS may also be more susceptible to seborrheic dermatitis due to the weakened immune system. Neurological disorders such as dementia and stroke may also increase the risk of seborrheic dermatitis due to changes in the nervous system that affect the skin.
| Treatment | Description | Population |
|---|---|---|
| Topical antifungal agents | Inhibits the growth of Malassezia, the yeast that contributes to seborrheic dermatitis | All populations |
| Topical corticosteroids | Reduces inflammation and itching | All populations |
| Calcineurin inhibitors | Reduces inflammation by inhibiting the immune response | All populations |
| Oral antifungal agents | Prescribed in severe cases | All populations |
| Topical keratolytics | Reduces scaling and flaking | All populations |
| Pimecrolimus cream | Effective for facial seborrheic dermatitis in adults | Adults |
| Mild topical corticosteroids | Preferred over stronger formulations to avoid skin thinning and scarring | People with skin of color |
Treatment Options for Seborrheic Dermatitis in Diverse Populations
Treatment options for seborrheic dermatitis may vary depending on the age, ethnicity, and medical history of the patient. Topical antifungal agents such as ketoconazole, ciclopirox, and selenium sulfide are commonly used to treat seborrheic dermatitis. These agents work by inhibiting the growth of the yeast Malassezia, which is thought to contribute to the development of seborrheic dermatitis.
Topical corticosteroids such as hydrocortisone and desonide may also be used to reduce inflammation and itching. Calcineurin inhibitors such as tacrolimus and pimecrolimus are also effective in reducing inflammation. These agents work by inhibiting the immune response that causes inflammation on the skin.
In severe cases, oral antifungal agents such as fluconazole and itraconazole may be prescribed. Topical keratolytics such as salicylic acid and sulfur may also be used to reduce scaling and flaking.
It is important to note that some treatments may be more effective in certain populations than others. For example, a study published in the Journal of Drugs in Dermatology found that pimecrolimus cream is effective for facial seborrheic dermatitis in adults. In people with skin of color, mild topical corticosteroids may be preferred over stronger formulations to avoid skin thinning and scarring.
FAQs
What causes seborrheic dermatitis?
The exact cause of seborrheic dermatitis is unknown, but it is thought to be related to an overgrowth of a yeast called Malassezia on the skin. Other factors that may contribute to seborrheic dermatitis include hormonal changes, stress, certain medical conditions, and a weakened immune system.
Is seborrheic dermatitis contagious?
No, seborrheic dermatitis is not contagious.
Can seborrheic dermatitis be cured?
Seborrheic dermatitis is a chronic condition that may require ongoing management. Although there is no cure for seborrheic dermatitis, it can be effectively managed with proper treatment.

Insider Tips
- Seborrheic dermatitis is a chronic condition that requires ongoing management. It is important to work with an interprofessional healthcare team to develop an effective treatment plan.
- Patients with skin of color may require different treatment approaches than patients with lighter skin tones. Mild topical corticosteroids may be preferred over stronger formulations to avoid skin thinning and scarring.
- Controlling the skin microbiome may help treat and prevent seborrheic dermatitis. Recent research shows that the skin microbiome is associated with seborrheic dermatitis, and interventions such as probiotics and topical microbiome modulators may be effective in restoring skin homeostasis in patients with seborrheic dermatitis.

